U-M researchers develop a personalized RNA therapeutic used to treat twins with an ultra-rare form of Batten disease
September 25, 2024
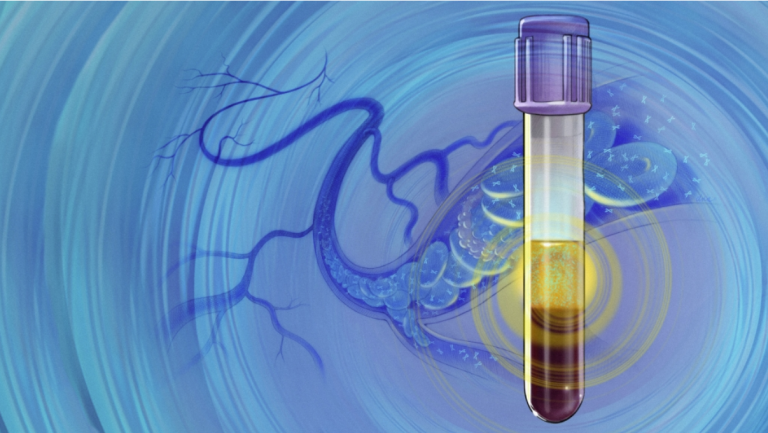
ANN ARBOR, Mich. — In a remarkable display of bench to bedside science, a therapeutic developed by U-M’s Michelle Hastings, Ph.D., is now being used to treat twin girls with a rare form of juvenile Batten disease.
Hastings, who is the Pfizer Upjohn Research Professor of Pharmacology, Director of RNA Therapeutics at the U-M Center for RNA Biomedicine, has been working on the drug platform, called antisense oligonucleotides (ASO), for nearly twenty years.
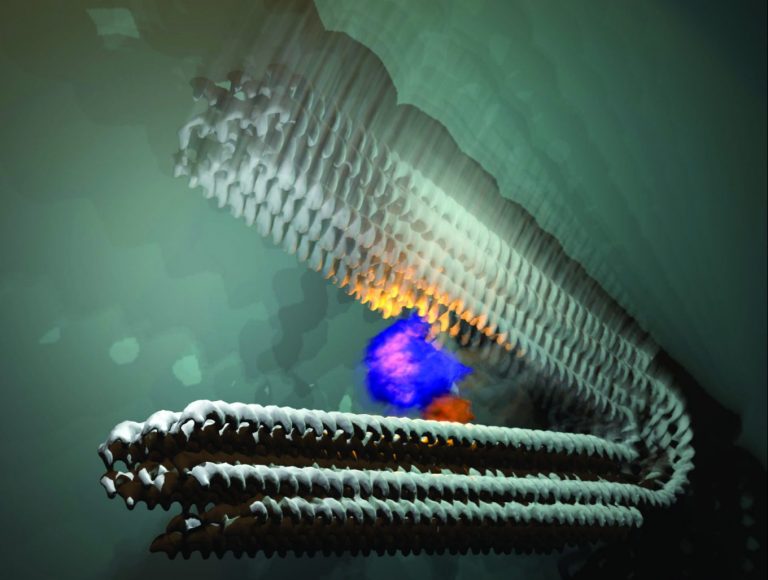
ASOs, Hastings explained, can be used to “fix” genes with specific mutations, like the CLN3 mutation responsible for the girls’ disease.
Batten (CLN3) disease is an inherited, fatal pediatric neurodegenerative disorder with no treatment that directly addresses the cause of the disease. After four to seven years of normal development, children with this condition develop vision impairment, intellectual disability, movement problems, speech difficulties, and seizures, which worsen over time until premature death sometime between their teens and thirties.
Because of her expertise, Hastings, along with senior postdoctoral fellow Jessica Centa, Ph.D., were approached by the ForeBatten Foundation, a nonprofit organization created in 2017 by Karen and David Kahn shortly after their twin daughters Amelia and Makenzie were diagnosed with CLN3 Batten disease caused by a very rare CLN3 c.569dupG mutation.
The U-M team conducted basic scientific research on the common mutation found in ~85% of CLN3 Batten disease and later, also on the mutation unique to the twins.

Pfizer Upjohn Research Professor of Pharmacology, Director of RNA Therapeutics at the U-M Center for RNA Biomedicine
ASOs of the type used by Hastings for CLN3 Batten, are small pieces of synthetic RNA molecules that are essentially reverse copies of genetic material. They bind to specific pieces of RNA in a cell much like one side of a piece of Velcro attaching to its mate, to modify how the gene is being expressed. These ASO molecules can be injected and taken up by the cells in the body.
“We and other investigators have been targeting and designing antisense therapeutics to target both rare and common diseases for which there is a known genetic cause,” said Hastings.
Realizing the potential of antisense therapeutics, the Food and Drug Administration (FDA) refined their regulations for so-called investigational new drugs (IND), clearing the way for Hastings and the ForeBatten Foundation to develop a highly targeted therapeutic for the twins.
“ASOs hold promise as therapeutics because, when carefully designed, they can be safe and also developed rapidly for targeted therapies for specific mutations,” said Hastings.
Hastings and the ForeBatten Foundation team received notification from the FDA in May 2024 that the clinical investigation for the ASO developed for the girls’ mutation — dubbed Zebronkysen after the girls’ beloved stuffed animals, Zebra and Monkey — may proceed.
Said Hastings, “This effort was realized through a cooperative effort of scientists, clinicians, and an experienced drug development team. We are enthusiastic about the potential for this ASO to help the girls and also about the trail we are blazing, which unlocks new possibilities for personalized RNA-based treatment solutions.”
Guided by the ForeBatten Scientific Advisory Board, the drug development team included members of the Hastings Lab at U-M and Rosalind Franklin University of Medicine and Science, The University of North Carolina School of Medicine Department of Neurology, Vanguard Clinical, BioDev Consulting, Keane Consulting, SciLucent, INRS Quebec, Sanford Research and others.
Hastings said the current findings give hope for an ASO-based therapy for the more common Batten mutations in the near future.
Her ultimate goal is to help investigators within the U-M Center for RNA Biomedicine, across campus and beyond, to develop potential therapeutic molecules that they can design from their own fundamental research to apply to new disease treatments.

Michelle Hastings, Ph.D., presents an overview of the RNA Therapeutics Initiative at the University of Michigan
“At the end of the day I’m a basic scientist and what we accomplished was bringing this technology to the clinic with the help of a collaborative team,” she said.
“I think it highlights that researchers and clinicians can be the drivers of a path forward for the rapid development and synthesis of frontline therapeutics.”
As for the young patients, they began therapy with Zebronkysen in June 2024, at the University of North Carolina Medical School. The treatment is being overseen by UNC Associate Professor of Neurology Yael Shiloh-Malawsky, M.D.
Karen and David Kahn have done everything possible to ensure their girls have the best quality of life and happiness, including making an informed and rational decision to pursue this treatment.
They express, “We have confidence in the researchers and scientific advisors who have been with us since the diagnosis. While it is too soon to determine how Zebronkysen will affect the girls’ disease trajectory, we find great excitement and comfort in accomplishing what we set out to do seven years ago.”
To learn more about ForeBatten Foundation, visit https://www.forebatten.org/.
In May 2022, Yael Shiloh-Malawsky, M.D., a neurologist at the UNC School of Medicine, met two new patients combatting a rare and fatal neurodegenerative disorder called Batten disease. With help from UNC, the twin girls were able to get personalized treatment developed by Dr. Michelle Hastings, RNA Therapeutics Initiative Director, Center for RNA Biomedicine at the University of Michigan, from bench to bedside in record time.
Video courtesy of UNC School of Medicine.